
your health is our priority.
As urologists, our modern approach to collaborative healthcare prioritises our patients with:
- Comprehensive urological care catered for you
- Shared team model with collective expertise
- State of the art medical technology
- End to end patient first care
- Clinics conveniently located throughout all of Auckland’s regions
- Fast access with short wait times
Services.
Cancer care
Cancer care
The uncertainty of a diagnosis can be stressful as you look for answers or treatment as soon as possible. With comprehensive on-site testing and a rapid diagnosis pathway, we provide urgent care for all urology cancers including prostate, bladder, kidney, testicular, and penile cancers. Shared knowledge between our surgeons and with our patients is a priority, our patients are empowered to make decisions and feel in control of their health and life.
Trusted Patient Resources
We encourage patients and families to learn from reputable New Zealand organisations that provide information and support:
-
Prostate Cancer Foundation of New Zealand – Offers education, peer support groups, and resources for men and their families following prostate cancer diagnosis and treatment.
-
Cancer Society of New Zealand– Provides information about living with cancer, treatment options, counselling services, and local support centres throughout the country.
These links are provided for general educational purposes and do not replace specialist medical advice.
Concerned about cancer?
Prostate Cancer
Prostate Cancer
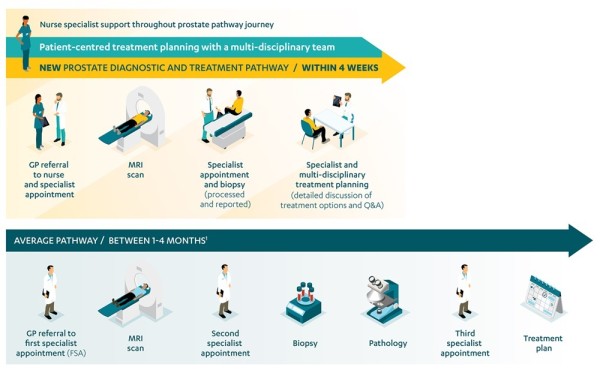
Our team provides comprehensive prostate cancer assessment and treatment — from early detection to advanced management.
Using modern diagnostics such as MRI fusion biopsy and active surveillance protocols, we tailor every plan to the individual.
When surgery is required, our surgeons offer robotic and minimally invasive techniques designed for precision, safety, and rapid recovery.
Learn more about our dedicated Prostate Cancer Clinic.
Concerned about prostate cancer?
Blood In The Urine
Blood In The Urine
Seeing blood in the urine — even once — should always be investigated.
Common causes include infection, kidney or bladder stones, inflammation, or, in some cases, cancers of the bladder, kidney, or prostate.
At Urology Institute, patients with suspected haematuria are assessed through our urgent investigation pathway.
When your referral indicates an urgent haematuria assessment, we will:
-
Arrange an urgent ultrasound or CT scan to evaluate the urinary tract.
-
Fast-track your appointment for a flexible cystoscopy (a detailed bladder examination performed in our clinic).
This coordinated approach ensures investigations are completed promptly and that results and treatment options are discussed without delay.
If your GP has requested urgent haematuria assessment, please forward the referral — our team will prioritise scheduling to ensure timely care.
Concerned about blood in the urine?
Urinary Incontinence
Urinary Incontinence
Incontinence affects thousands of New Zealanders every year — but it is treatable. At Urology Institute we assess the underlying causes and tailor treatment plans that may include lifestyle change, bladder training, medical therapy or minimally invasive surgery.
Whether you’re experiencing leakage when you laugh, cough or exercise, or leakage without warning, our team is here to restore your confidence, comfort and quality of life.
Patient support resource:
Visit Continence New Zealand for trusted information, educational resources and support groups.
https://www.continence.org.nz (opens in new window)
Concerned about urinary incontinence?
Pelvic Organ Prolapse
Pelvic Organ Prolapse
Pelvic organ prolapse occurs when the muscles and tissues that support the bladder, uterus, or bowel weaken, allowing one or more organs to drop into the vaginal space.
It is a common condition that can cause a feeling of pressure, bulging, or discomfort — especially after childbirth or with age.
At Urology Institute, our specialists provide careful assessment and a full range of treatments for prolapse.
We offer both non-surgical options (pelvic floor therapy, pessary fitting, lifestyle and physiotherapy support) and surgical repair when needed — using minimally invasive or robotic techniques for faster recovery and durable results.
Our goal is to help you feel comfortable, confident, and in control again — with treatment tailored to your needs and lifestyle.
Patient support resource:
For information and community support, visit Continence New Zealand, which offers excellent education on prolapse and pelvic floor health:
Urinary Tract Infections
Urinary Tract Infections
Recurrent urinary tract infections can have a major impact on quality of life.
At Urology Institute, we investigate the underlying cause of recurrent infections and work with patients to reduce their frequency and severity through evidence-based prevention strategies.
Our specialists provide assessment to rule out structural or functional causes (such as bladder emptying issues, stones, or prolapse) and tailor a prevention plan suited to each individual.
Options may include:
-
Lifestyle and behavioural measures – improving hydration, timed voiding, and post-intercourse hygiene.
-
Preventive therapies – your GP or specialist may discuss options such as:
-
Uromune® – an oral vaccine that helps the immune system build resistance against the bacteria most often responsible for UTIs.
-
D-mannose – a naturally occurring sugar that may help prevent certain bacteria (especially E. coli) from adhering to the bladder wall.
-
Hiprex® (methenamine hippurate) – a non-antibiotic urinary antiseptic used to prevent recurrent infections in suitable patients.
-
These treatments may not be appropriate for everyone. Patients should discuss suitability, interactions, and availability with their GP or urologist before starting any new therapy.
Our goal is to reduce infection frequency and reliance on antibiotics, helping patients maintain long-term bladder health and comfort.
Concerned about urinary tract infections?
book an appointment